A Fatal Case of Levamisole-Induced Vasculitis
Samuel Han, Andrew Hsu, Rosa Bui and Richard T Ellison III
Samuel Han1*, Andrew Hsu1, Rosa Bui1 and Richard T Ellison III2
1Department of Internal Medicine, University of Massachusetts Medical School, Worcester, MA 01655, USA
2Department of Infectious Disease, University of Massachusetts Medical School, Worcester, MA 01655, USA
- *Corresponding Author:
- Samuel Han
Department of Internal Medicine, University of Massachusetts
Medical School Worcester, MA 01655, USA
Fax: (774)-442-6781
E-mail: Samuel.Han@umassmemorial.org
Received date: December 14, 2015; Accepted date: February 10, 2016; Published date: February 18, 2016
Citation: Han S, Hsu A, Bui R, et al. A Fatal Case of Levamisole-Induced Vasculitis. Skin Dis Skin Care. 2016, 1:1
Copyright: © 2016 Han S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Background
Levamisole is an antihelminthic agent used mainly by veterinarians that is now commonly used as an adulterant in cocaine [1]. Numerous case reports have connected levamisole with vasculitis and neutropenia [2,3]. Our case focuses on a patient who used weekly cocaine contaminated with levamisole and developed necrosis of the skin in her lower extremities, abdomen, and lower back. To our knowledge, this is also the only case of levamisoleinduced vasculitis with leukocytosis, as neutropenia appears to be the typical finding.
Case Presentation
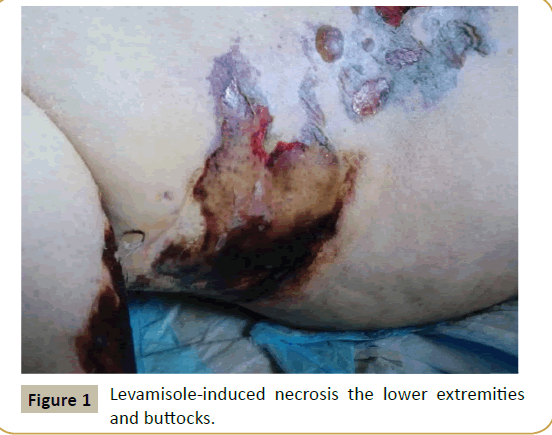
We present a 30 year old female with history of hypothyroidism and alcohol abuse who presented to the hospital with complaints of ecchymoses on bilateral thighs associated with burning and hypersensitivity to touch and a 3 day history of jaundice. The patient also noted a 3-week duration of generalized weakness and dizziness, while also noting 8 weeks of heavy vaginal bleeding. The patient used weekly cocaine, the last use was 4 days prior to admission, and consistently drank 40 ounces of malt liquor per day. On examination, vital signs were stable, but the patient was ill-appearing and jaundiced. Detailed skin examination revealed several deep red to violaceous ecchymoses, ranging in size from about 3-10 cm in diameter, on the bilateral lower extremities (Figure 1). Several had large central serosanguineous-filled bullae and some had overlying erosions. Similar lesions were also found on her buttocks and lower abdomen. Other physical examination revealed multiple focal, blanching telangiectasias on the upper chest.
Investigations
Laboratory findings revealed leukocytosis with a white blood cell (WBC) count of 23,800 cells/μL, a hemoglobin and hematocrit (H/H) of 3.4 (g/dL)/11.3 (%), lactate of 4.3 mmol/L, sodium of 125 mmol/L, creatinine of 4.53 mg/dL and elevated liver function tests including a total bilirubin of 8.1 mg/dL, AST of 117 IU/L and ALT of 58 IU/L. Antinuclear cytoplasmic antibody (ANCA) was found to be negative and IgM cardiolipin antibody was also negative (2.9 U/mL).
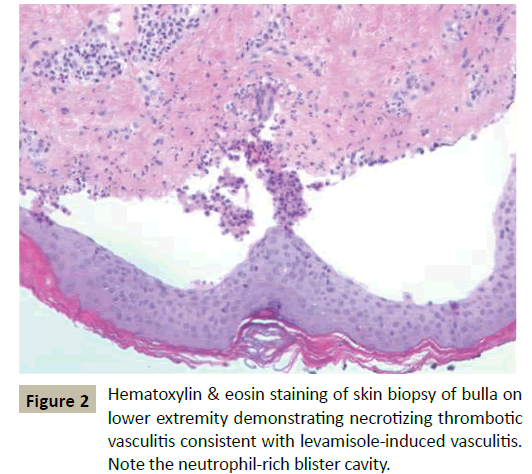
The patient had a urine toxicology screen that was positive for cocaine and gas-chromatography mass spectrometry (GCMS) that was positive for levamisole. Biopsy of the lower extremity lesions was consistent with necrotizing thrombotic vasculitis with associated findings of fibrinoid necrosis of small vessels, neutrophil leukocytoclasia, and extravasated erythrocytes and intravascular occlusive thrombi involving the superficial dermis to the subcutis (Figure 2).
Treatment
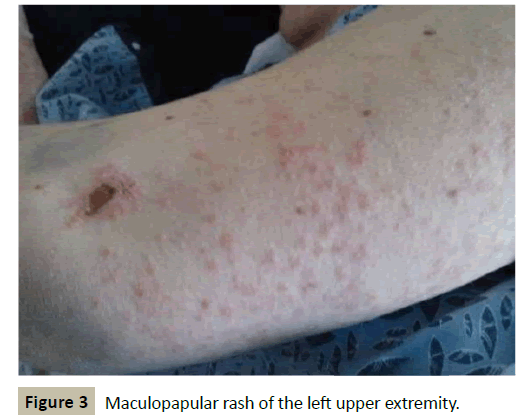
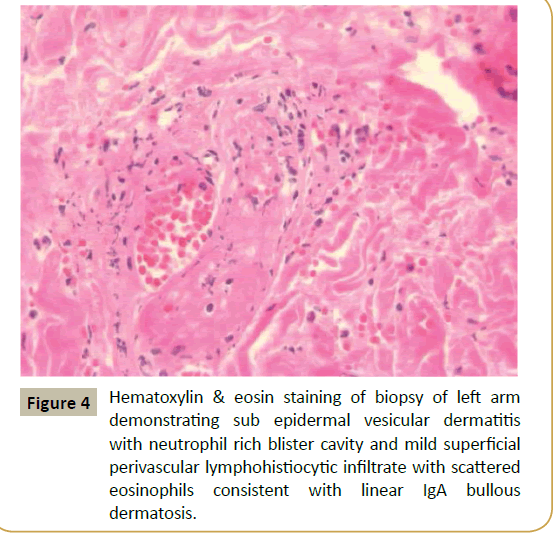
The patient initially received 7 units of packed red blood cells (pRBC) and was initiated on vancomycin for one out of four blood culture bottles growing Methicillin-sensitive Staphylococcus aureus (MSSA) and a urine culture growing 100,000 colonies of Staphylococcus aureus. The patient received only 2 days of vancomycin therapy, but shortly after discontinuation began developing multiple flat rust to pink-colored macules and papules, approximately 1-3 mm in size and grouped into irregular patches, on the bilateral upper forearms and upper back (Figure 3). Biopsy of these lesions showed subepidermal vesicular dermatitis with neutrophil rich blister cavity and mild superficial perivascular lymphohistiocytic infiltrate with scattered eosinophils, consistent with a linear IgA reaction to vancomycin (Figure 4).
The patient’s lower extremity skin findings progressed to become large shallow denuded ulcers and bullae in stellate arrangements, some of which had a dusky color to them, that were tender and had an indurated texture to them. They extended from the bilateral ankles up to the upper thighs and buttocks, while also involving her inferior anterior abdomen and back. The patient was treated with a tapering course of prednisone, which very slowly improved her lesions.
Outcome and Follow-Up
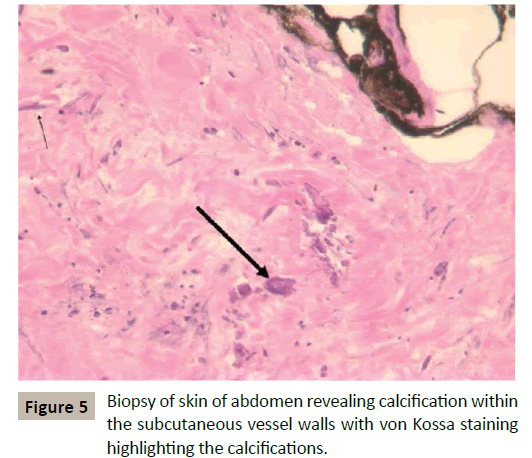
Our case has an unfortunate ending as our patient eventually expired a little over 2 months after being initially admitted. After having initially been discharged to a long-term care facility, the patient was brought back to the emergency department with septic shock complicated by acute respiratory failure, acute renal failure, and liver failure. She was found on imaging to have bilateral lower lobe lung consolidations, diffuse colitis, severe osteopenia, and multiple compression fractures in her spine. Due to her worsening wounds, she received two debridement procedures with wound cultures growing Pseudomonas aeruginosa and biopsy showing calciphylaxis (Figure 5). Despite aggressive wound management and extensive volume resuscitation, the patient eventually succumbed to the septic shock.
Discussion
First described in the 1970s, levamisole-induced vasculitis produces a syndrome of vasculitis that most commonly involves the lower extremities, but has also been found to involve the ears, the upper extremities, face, and trunk [4]. In terms of laboratory findings, up to 60% of patients have been found to have neutropenia [3]. Patients may also present with ANCA abnormalities, with perinuclear ANCA (p-ANCA) found to be elevated in up to 88% of patients. Additionally, cytoplasmic ANCA (c-ANCA), anti-myeloperoxidase (anti-MPO), anti-proteinase 3 (anti-PR3), and anti-neutrophil antibody (ANA) have also commonly found to be elevated [3]. Histologically, biopsy results typically demonstrate thrombocytic vasculopathy, vasculitis, or a combination of thrombosis with a vasculitis [3].
In terms of skin findings, our patient had typical findings with the majority of her vasculitis involving the lower extremities, but also including the trunk. Her skin findings were complicated by her showing stigmata of liver disease, including jaundice and telangiectasias over her chest. Initially, when the patient developed a rash on her upper extremities, this was also thought be sequelae of the vasculitis; however, the different color and maculopapular nature of the rash suggested a second process and biopsy indeed confirmed a diagnosis of a linear IgA reaction to the vancomycin the patient had received for 2 days in her initial therapy (Figure 4). Once the patient was started on treatment with prednisone, the lower extremity lesions began to slowly improve.
While displaying classic skin findings and typical histological findings on biopsy, our patient did not demonstrate usual laboratory data associated with levamisole-induced vasculitis. Our patient was tested for p-ANCA and c-ANCA and was found to be negative for both. She was also found to be negative for ANA, rheumatoid factor (RF), and IgM cardiolipin antibody. Levamisole has been shown to have several immunomodulating effects; however, despite various repeat testing, our patient displayed none of the antibodies one would expect. As part of a work-up for her liver disease, the patient had also been tested for the various autoimmune liver conditions, all of which was negative.
There are some potential explanations of the leukocytosis, as the patient was initially treated for an infection. The patient did grow Staphylococcus aureus in her initial urine culture, and had one out of four blood culture bottles positive for Staphylococcus aureus. However, after 1 week of antibiotic therapy, the patient continued to have a leukocytosis and her WBC count never went below 15,600 cells/μL, and remained elevated in the 20,000+ range for the following 2 months until her expiration. After the initial blood and urine cultures, all subsequent cultures did not demonstrate any microbial growth. Another potential confounder was the presence of her liver disease. The patient presented with what appeared to be alcoholic hepatitis. Alcoholic hepatitis may present with moderate leukocytosis (WBC < 20,000 cells/μL), and one study showed a mean WBC count of 11,000 [6,7]. However, as mentioned, our patient had a persistently elevated WBC count greater than 20,000 cells/μL. In very rare cases, alcoholic hepatitis may present with a leukemoid reaction with a WBC count that ranges from 57,000 to 129,000, which was not the case in our patient [8]. An alternative explanation for the persistent leukocytosis involves the use of steroids as the treatment – oral prednisone, the typical treatment for levamisole-induced vasculitis, was used for an extended duration in our patient due to the slow nature of her healing. As known, glucocorticoids are associated with a low-grade neutrophilia and resultant leucocytosis [9]. However, it is difficult to account for the prolonged nature of the high leukocytosis on the basis of the steroid use alone. The leukocytosis was likely a cumulative effect of all the factors mentioned above, but represents a novel finding in patients with this vasculitis.
Unfortunately, this patient’s morbidity and mortality likely stemmed from the levamisole-induced vasculitis. Given the extensive and poorly healing nature of the wounds from the vasculitis, the patient eventually developed an infection in the wounds, which resulted in septic shock and its various complications, including renal failure, liver failure, and respiratory failure. The renal failure most likely led to the development of calciphylaxis as well, and despite aggressive debridement therapy, the patient was unable to recover from these insults. To our knowledge, this is the only known case of mortality resulting from complications of levamisole-induced vasculitis and this case highlights the need for development of additional treatment options beyond prednisone. Furthermore, this case reinforces the importance of supportive care as the patient demonstrated initial improvement with around-the-clock wound care management while hospitalized. Once the patient was discharged to a rehabilitation facility, she did not receive adequate wound care management, which likely predisposed her to receiving wound infections.
Learning Points
Levamisole-induced vasculitis is an increasingly common syndrome and should be considered in patients with findings of cutaneous vasculitis in the setting of cocaine use.
Levamisole-induced vasculitis typically leads to elevations in neutrophils, p-ANCA, c-ANCA, anti-myeloperoxidase, IgM cardiolipin, anti-proteinase 3, and/or ANA. However, levamisoleinduced vasculitis may present with leukocytosis, as in this case.
Histologically, biopsy results typically demonstrate thrombotic vasculopathy, small-vessel vasculitis, or a combination of both.
References
- Amery WK, Bruynseels JP (1992)Levamisole, the story and the lessons. Int J Immunopharmacol14: 481-486
- Arora NP, Jain T, Bhanot R, Natesan SK(2012)Levamisole-induced leukocytoclasticvasculitis and neutropenia in a patient with cocaine use: An extensive case with necrosis of skin, soft tissue, and cartilage. Addict SciClinPract 7:19
- Abdul-Karim R, Ryan C, Rangel C, Emmett M (2013) Levamisole-induced vasculitis. Proc (BaylUniv Med Cent)26:163-165
- Macfarlane DG, Bacon PA (1978)Levamisole-induced vasculitis due to circulating immune complexes. Br Med J 1(6110):407-408
- Thompson JS, Herbick JM, Klassen LW (1980) Studies on levamisole-induced agranulocystsis. Blood 56: 388-96
- Stewart S, Prince M, Bassendine M (2007) A randomized trial of antioxidant therapy alone or with corticosteroids in acute alcoholic hepatitis. J Hepatol47:277
- Nguyen-Khac E, Thevenot T, Piquet MA(2011) Glucocorticoids plus N-acetylcysteine in severe alcoholic hepatitis. N Engl J Med365:1781
- Mitchell RG, Michael M, Sandidge D (1991) High mortality among patients with the leukemoid reaction and alcoholic hepatitis. South Med J 84:281
- Dale DC, Fauci AS, Guerry D IV, Wolff SM (1975) Comparison of agents producing a neutrophilicleukocytosis in man. Hydrocortisone, prednisone, endotoxin, and etiocholanolone. J Clin Invest 56:808
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences