A Case of Kerion Due to Trichophyton mentagrophytes: Neglected Post- Traumatic Infections?
Ming-Kai JI and Cheng B*
Ming-Kai JI and Cheng B*
Department of Dermatology, The First Affiliated Hospital, Fujian Medical University, China
- *Corresponding Author:
- Bo Cheng
Department of Dermatology
The First Affiliated Hospital
Fujian Medical University
Fuzhou 350004, China
Tel: +86-0591-87981393
Fax: +86-0591-83318716
E-mail: chengbo630415@126.com
Received Date: March 22, 2017; Accepted Date: April 06, 2017; Published Date: April 10, 2017
Citation: Ming-Kai JI, Cheng B. A Case of Kerion Due to Trichophyton mentagrophytes: Neglected Post-Traumatic Infections? Skin Dis Skin Care. 2017, 2:1.
Copyright: © 2017 Ming-Kai JI, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
A healthy 11-year-old boy with a kerion celsi, caused by Trichophyton mentagrophytes, probably acquired from an injury on the scalp. The lesions had started as papulonodules that had been diagnosed as a bacterial abscess. Nevertheless, they had not responded to systemic antibacterial treatment for 14 days. Finally, successful treatment was performed by means of oral application of itraconazole 5 mg/kg/day for 12 weeks. The boy was left with scarring alopecia.
Keywords
Trichophyton mentagrophytes; Dermatology; Granulocytes; Papulonodules
Case Report
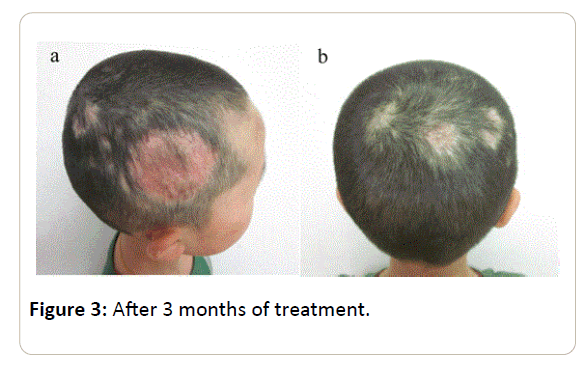
A formerly health 11-year-old boy was presented at the dermatology department with a 2-month history of an inflammatory mass on the scalp after an injury. The lesions had started as papulonodules, developed a boggy swelling studded with pustules and squamous lesions that had been diagnosed as skin infection by local clinics. They had been treated with systemic ceftriaxone sodium 50 mg/kg/day for 2 weeks. Besides, wounds were rinsed twice every day and dressed with ethacridin solution topically. Although a painless swelling progressed on the scalp, cervical lymph nodes were not swollen and general symptoms such as fever did not occur. Physical examination at the department showed a boy in good general condition. His head was covered with big crusts full of hairs, papulonodules and blood. The boy’s hair was cut showing a purulent infection covering an 8 × 10 cm large area of the scalp with necrotic defects. A presumptive diagnosis of kerion celsi was made in our patient. Skin scrapings for mycological culture and swabs for bacteriological culture were taken. The result confirmed a dermatophyte infection with Trichophyton mentagrophytes, but no bacteria. Skin biopsy showed an inflammatory reaction with neutrophilic granulocytes infiltrates consistent with kerion celsi, as well as hyphal threads with the periodic acid-Schiff reaction and Gomori Methenamine Silver stain. A 3-month course of oral itraconazole 5 mg/kg/day resulted in the successful resolution of symptoms, mycologic clearance and scarring alopecia (Figures 1-3).
Discussion
Tinea capitis is a common fungal infection in pre-pubertal children that should be considered in any type of scalp lesion. The presenting symptoms vary widely, ranging from the more typical scaling lesions to large painful inflammatory masses, the latter often with crusting and purulent discharge, called kerion celsi [1,2].
Causative fungi are usually divided into three groups: Zoophilic, kerion celsi and geophilic. Mycoticinfection in humans by zoophilic dermatophytes are commonly caused by Microsporumcanis and Trichophyton species.
Although effective antimycotic drugs are presently available, microscopic examination of a potassium hydroxide preparation of material obtained by scraping is the decisive examination for the early establishment of an effective therapeutic regimen.
Kerion celsi is the result of an intense hypersensitivity reacting from a dermatophytic infection caused by T-cell and is most often seen in zoophilic fungal infections, with a more uncommon symptom, a severe inflammatory reaction and some devastating consequences [3,4].
In our patient, Kerion celsi has occurred after a trauma, which suggests that in this case the acquisition of the fungus may be due to the injury rather than animal origin. Another problem is the misdiagnosis of kerion celisi as a bacterial abscess and the subsequent surgical treatment made the presenting symptom develop secondarily and left permanent scarring alopecia [5].
Early diagnosis may avert unnecessary and inappropriate antibiotic therapy; avoid the development of Kerion celsi, with sometimes devastating consequences.
Ethical Statement
On behalf of the authors, and with their permission, I declare that:
1. The material has not been published in whole or in part elsewhere.
2. The paper is not currently being considered for publication elsewhere.
3. All authors have been personally and actively involved in substantive work leading to the report, and will hold themselves jointly and individually responsible for the content.
4. For publication as “Research Paper” in Clinics in Dermatology is approved by all authors and tacitly by the responsible authorities where the work was carried out, and if accepted, it will not be published elsewhere in the same form, in English or in any other language, without the written consent of the copyright-holder.
References
- Zhang H, Ran Y, Liu Y (2009) Arthroderma vanbreuseghemii infection in three family members with kerion and tinea corporis. Med Mycol 47: 539-544.
- Nenoff P, Handrick W, Krüger C (2012) Dermatomycoses due to pets and farm animals:neglected infections? Hautarzt 63: 848-858.
- Isa IR, Arenas R, Isa M (2010) Inflammatory tinea capitis: kerion, dermatophytic granuloma, and mycetoma. Clin Dermatol 28: 133-136.
- Proudfoot LE, Morris JR (2012) Images in clinical medicine, Kerion celsi. N Engl J Med 366: 1142.
- He XDÃÆïÃâüÃâà âRan YPÃÆïÃâüÃâà âLi FZ (2006) Kerion Misdiagnosed as abscess on scalp which is responsless to antibiotics and skingrafting: two case reports. Chinese J Mycol pp: 1330-333.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences